The Case for a Robust Home Dialysis Program
There are many reasons to embrace home therapies, and not just for the youngest and healthiest of the dialysis patient population. It's time to expand our programs and even our concept of "home" to give patients more control over their lives, reduce hospitalizations, increase survival, and lower costs. To reach its 2022 goal of treating more than 15 percent of patients in a home setting, Fresenius Medical Care North America (FMCNA) is focusing on reducing patient burden through technological innovations, physician education, family support, transitional care dialysis units, and expanded telemedicine platforms.
In the United States, in-center hemodialysis has been the face of dialysis since the late 1970s. Even today, amid a generational low in utilization of in-center hemodialysis, only 12 percent of patients dialyze at home. However, throughout the healthcare industry, person-centered care and empowered self-care is on the rise. In dialysis, technological advancements are bringing care home. Improvements in machine technology and connected health have made home dialysis simpler and more portable, thus increasing access for patients. Future device evolution will continue to increase safety, communication, and portability, and reduce burden while improving the care delivery process.
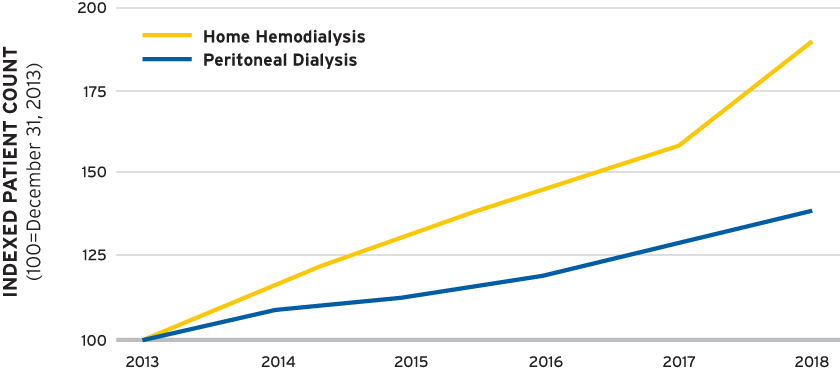
Fresenius Kidney Care has embraced the move to the home. Compared to five years ago, the number of Fresenius Kidney Care patients on home hemodialysis (HHD) and peritoneal dialysis (PD) has increased by 90 percent and 39 percent, respectively (Figure 1).
FIGURE 1 | Relative growth of home therapies
Home and self-care dialysis treatments are the quintessential path to empower patients and families, allowing patients the freedom to manage their treatments and disease. PD allows needleless daily dialysis, preserves residual renal function, and has early survival benefits. HHD eases delivery of more frequent dialysis (MFD) therapies in a cost-efficient manner. Studies show MFD of greater than five days per week improves blood pressure control with reduced medications and improves overall volume management. MFD can reduce the intradialytic volume complications of high ultrafiltration rates, cardiac stunning, prolonged recovery rates, and hypotension (Figure 2). In studies, MFD has been shown to address the interdialytic volume complications of left ventricular hypertrophy, hypertension, and congestive heart failure. Home therapies performed effectively address cardiac status and common complications of dialysis, reduce hospitalizations, increase survival, and lower costs. Most importantly, home therapies allow patients to succeed in living better lives with their families.
FIGURE 2 | Ultrafiltration rates (UFR) and recovery time in dialysis and effect of more frequent dialysis
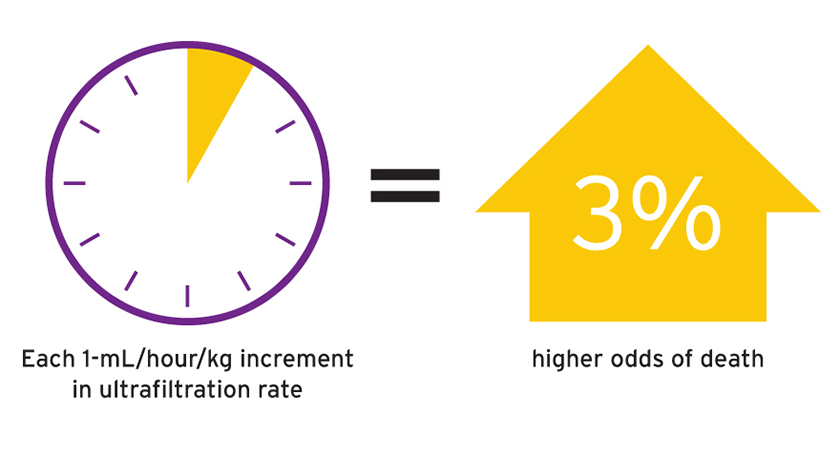
Source: Assimon MM, et al. Ultrafiltration rate and mortality in maintenance hemodialysis patients. Am J Kidney Dis 2016;68(6):911-22.
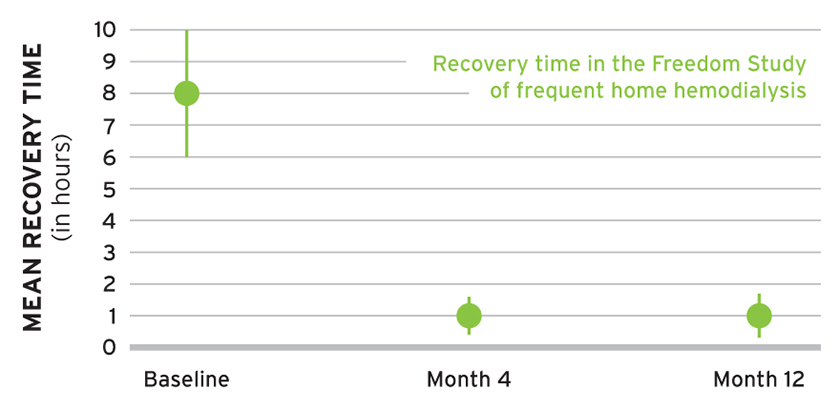
Source: Jaber BL, et al. Effect of daily hemodialysis on depressive symptoms and postdialysis recovery time: interim report from the FREEDOM (Following Rehabilitation, Economics and Everyday-Dialysis Outcome Measurements) Study. Am J Kidney Dis 2010;56(3):531-9.
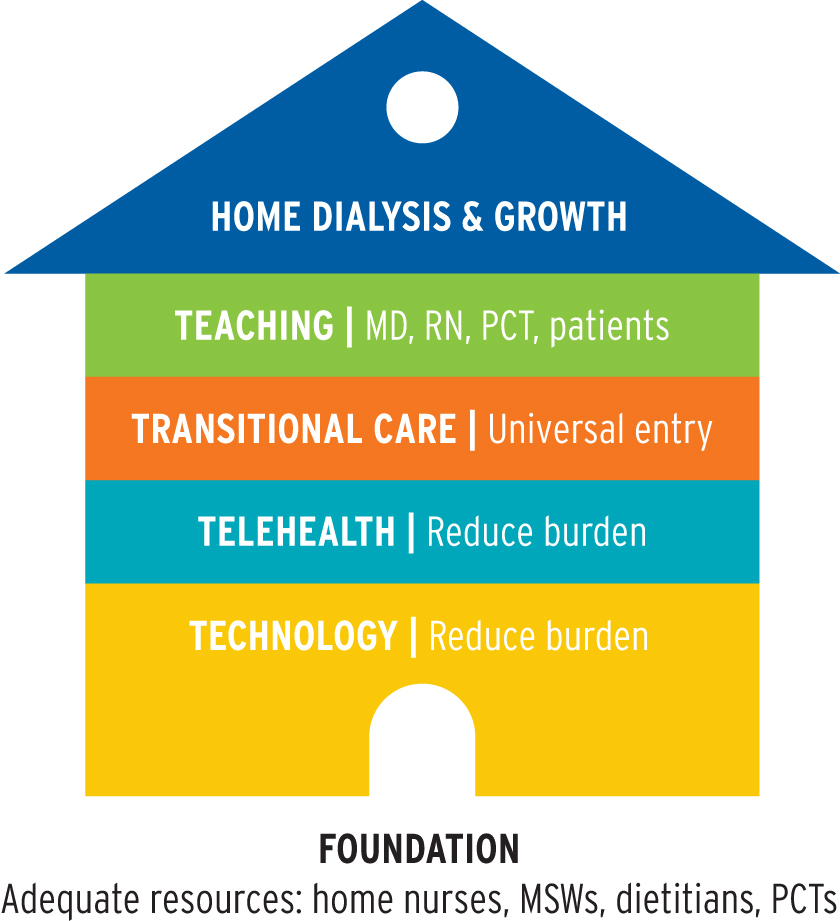
Chronic dialysis therapy has inherent burdens on patients, care providers, and families, often resulting in an unacceptable quality of life. Conventional hemodialysis has been called a "full-time job," making work impossible and travel difficult and compromising family time. The time spent on dialysis, transportation to and from the treatment center, and recovery (greater than six to eight hours for many patients) can exceed 30 hours per week. Well-supported home dialysis may actually reduce these burdens (Figure 3).
FIGURE 3 | Building blocks for successful growth in home dialysis
WHERE IS HOME?
At present, the "home" in home dialysis is typically a single-family home or an apartment, but the definition is expanding to be anywhere the patient chooses: a private residence, a travel destination, a skilled nursing facility, or even a community center. While dialysis in the actual home will remain the primary site of home therapies, the concept of a home without walls will evolve.
Patients are frequently limited by storage space, so delivery systems will need to advance to require less storage space. As PD devices mature with online fluid generation, storage needs will markedly decrease. Industry may have to consider better, more frequent delivery systems to meet patient needs, perhaps even an Uber-like, as-needed delivery system.
Examples of potential changes needed to improve access to home therapies include community centers and paid care partners. Denmark, New Zealand, and the United Kingdom have already begun to study the use of community centers for home patients.1 Patients come to the community center for self-care on a desired schedule, either in place of or in addition to care in their home locations. A community center solves the problem of not enough storage space and could prevent social isolation of dialysis that is only provided in the home. One could envision community dialysis centers offering access during televised events or shows to provide a community of dialysis patients with socialization opportunities. Creating virtual community centers with telemedicine allows for the building of social connections, bonding together, and looking out for one another—in short, building homes without walls and communities without borders.
Home dialysis need not be relegated to only self-care in the private residence. Development of paid partner models can bring home therapies to those who need assistance. Programs have been initiated in Canada to demonstrate the benefits and costs with HHD.2 Assisted PD is available in many high-income countries using health care workers and in some lower income countries using extended family members or domestic help, increasing access to person-centered care.3
While not truly a home therapy, self-care in-center dialysis units also empower and engage patients and can be a springboard to home therapies. Increasing in-center self-care should be a priority.
REMOVING BARRIERS AND IMPROVING RETENTION
There are very few contraindications to home therapy. Active drug or alcohol addiction and severe psychiatric illness without adequate support may make self-care impossible. Advanced age, low degree of education, significant comorbidities, language spoken, and illiteracy are perceived barriers that can be overcome with proper support and education tools. Given the right tools and support, patients can be empowered to control their own dialysis, medications, diet, and life.
Home dialysis access must be available for all patients, including those with a worse clinical prognosis. No longer can home therapies, particularly HHD, be offered to only the youngest and healthiest patients. PD and HHD, including MFD, improve the quality and quantity of life of the sickest and elderly patients. In fact, patients with more comorbidities can embrace home therapies. In the FREEDOM study, patients with the lowest quality of life at baseline exhibited the largest improvement during twelve months of frequent HHD.4 Given proper resources, these more challenging patients flourish on a home therapy.
Advancements in technology and telemedicine with both HHD and PD will improve access and decrease burden. Today, there are connected health platforms in use—including Baxter SharesourceTM, Fresenius Medical Care connected health platform, and the Nx2meTM platform from NxStage. These platforms have improved adherence, facilitated quicker training, and improved patient retention.5 Virtual clinic visits will decrease travel time for the patient and provide as-needed care. Telemedicine can improve adherence, reduce ER visits, and reduce hospitalization rates, resulting in lower costs and lower morbidity rates.
Growth of home therapies is dependent on the intake of new patients and improved patient retention. While technology changes and telemedicine will improve access and retention, patient and unit success depend on adequate resources in home dialysis units large enough to provide these resources at scale. In 2018, NxStage commissioned a survey of patients who had returned to in-center dialysis and a review of ten large US centers to explore best practices in training and retention (NxStage data is on file). Together, these studies suggest patient drops could be mitigated by engaged professionals with adequate resources, prescription adaptability (frequency, solo dialysis, and nocturnal dialysis), and clinic adaptability to meet the patient and partner needs.
NxStage's review of large home clinics found that the success of home dialysis programs varied by resources utilized. Successful units (measured as increased retention) invested in resources
and caregiver engagement. Specifically, better results occurred when utilizing professional nurses with the desire to grow home therapies, engaged and available social workers, dietitians knowledgeable about the changes in home therapies, and patient care technicians (PCTs) in the home unit. Appropriate addition of PCTs to perform tasks consistent with local scope of practice rules allowed more time for nurses to focus on patient education, care, and retention. In short, successful units have nursing champions with a strong interdisciplinary team with time committed to home.
Likewise, it is imperative to support physician champions in the home therapies with additional education and streamlining processes to improve efficiencies in the intake, education, and delivery of home therapies. Academic training in home therapies is thought to be lacking.6 FMCNA will provide novel training techniques to support physicians through this culture change. There is a commitment to building teams of physician champions with imbedded nursing champions.
PATIENT TRANSITIONS
All patients with end stage renal disease (ESRD) deserve adequate education on self-directed disease management, including:
- Disease education
- Dietary recommendations
- Medication management
- Modality options (transplant, peritoneal dialysis, home hemodialysis modalities, in-center care, and even hospice/palliative care)
While dialysis modality education is focused on CKD and in-center ESRD patients when they initiate therapy, there are special populations who need additional disease and modality education or reeducation to avoid immediate risks. Patients in transition have increased risk for hospitalizations, mortality, depression, and more outpatient care. These transitions include all transitions—the incident patient (new to ESRD), patients with failing PD or HHD therapy technique, patients losing transplant function, patients wanting to leave in-center, patients discharged from hospitals or transferred from/to skilled nursing facilities, and patients suffering from acute kidney injury requiring renal replacement. These pressure points are complicated by declining health, fear of transition, depression/grief, and, frequently, a lack of understanding of the illness and treatments.
Special attention is needed to help the PD patient transition to HHD as therapy technique fails. Nationally, 12,000 PD patients transitioned to hemodialysis in 2016, with less than 1 percent going to HHD. Education platforms need to be developed to help patients, physicians, and nurses understand the likelihood of transition and develop pathways of earlier transition to HD/HHD, which may reduce the increased morbidity seen with PD technique loss.
Transitional units, either in-center or free standing, will have the resources to educate on overall care and appropriate modality at the right time. They are more able to assist physicians with patients' ongoing medical issues with weight, blood pressure, medications, and even appropriate frequency of dialysis daily rather than monthly, to improve outcomes. Transitional units offer distinct advantages over traditional in-center units for these patients. Existing transitional unit experience has seen improvement in modality selection, patient satisfaction, and even improved adherence with in-center dialysis prescription.
Throughout the patient journey, needs change and transitions occur. Growth will be dependent on the ability to ease patients through transitions, define proper timing of transitions, and provide the right prescription for the right therapy every day.7,8
Meet Our Experts
MICHAEL A. KRAUS, MD, FACP
Associate Chief Medical Officer, NxStage, Fresenius Medical Care
Prior to working for NxStage, Michael Kraus held several positions and titles at Indiana University (IU) Health and Indiana University School of Medicine, including service line chief for IU Health Physicians, Kidney Diseases; and chief medical officer of IU Health Adult Dialysis Services. He is a leader in the field of short daily home hemodialysis and a well-published, internationally recognized invited speaker. He is a recipient of the Lifetime Achievement Award from the National Kidney Foundation of Indiana and of the Sagamore of the Wabash, the highest award presented to a citizen of Indiana.
DINESH CHATOTH, MD
Associate Chief Medical Officer, Fresenius Kidney Care
Dinesh Chatoth completed his fellowship in nephrology at the University of Texas Southwestern Medical Center in Dallas. He was an assistant professor of medicine and director of the dialysis program at the University of Arkansas for Medical Sciences. He has worked with the KDOQI workgroup for peritoneal dialysis and promotes home dialysis as a modality of choice for patients requiring renal replacement therapy. He oversees home therapy initiatives for the Medical Office and serves on the Fresenius Kidney Care Pharmaceutical and Therapeutics Committee.
References
- Walker RC, Howard K, Morton RL. Home hemodialysis: a comprehensive review of patient-centered and economic considerations. Clinicoecon Outcomes Res 2017 Feb 16;9:149-61. doi:10.2147/CEOR.S69340.
- Pierratos A, Tremblay M, Kandasamy G, et al. Personal Support Worker (PSW)-supported home hemodialysis: a paradigm shift. Hemodial Int 2017 Apr;21:173-9.
- Brown EA, Wilkie M. Assisted peritoneal dialysis as an alternative to in-center hemodialysis. Clin J Am Soc Nephrol 2016 Sep 7;11(9):1522-24. doi: 10.2215/CJN.07040716.
- Finkelstein FO, Schiller B, Daoui R, et al. At-home short daily hemodialysis improves the long-term health-related quality of life. Kidney Int 2012 Sep;82(5):561-9. doi: 10.1038/ki.2012.168.
- Weinhandl ED, Collins AJ. Relative risk of home hemodialysis attrition in patients using a telehealth platform. Hemodial Int 2018 Jul;22(3):318-27. doi: 10.1111/hdi.12621.
- Merighi JR, Schatell DR, Bragg-Gresham JL, Witten B, Mehrotra R. Insights into nephrologist training, clinical practice, and dialysis choice. Hemodial Int 2012 Apr;16(2):242-51. doi: 10.1111/j.1542-4758.2011.00649.x
- McCullough PA, Chan CT, Weinhandl ED, et al. Intensive hemodialysis, left ventricular hypertrophy, and cardiovascular disease. Am J Kidney Dis 2016; 68(5S1):S5-S14.
- Weinhandl ED, Collins AJ, Kraus MA. Ultrafiltration rates with more frequent home hemodialysis. Oral presentation at the Annual Dialysis Conference, Long Beach CA, March 2017.



