Choosing a Dialyzer
This article provides an overview of dialyzer characteristics that are important when choosing the right dialyzer for your patient. Key characteristics that influence dialyzer choice—including dialyzer materials, production methods, membrane surface area, and clearance parameters—are discussed here. While dialyzer choice may impact dialysis adequacy and patient outcomes, other factors including treatment time, vascular access function, and needle placement should be considered when optimizing treatment.
Synthetic membrane dialyzers made of synthetic polymers are the most common dialysis membranes in use today. There may be more than one type of polymer in a given synthetic dialysis membrane that may impart important characteristics (e.g., methallyl sulfonate mixed with polyacrylonitrile, and polyvinylpyrrolidone mixed with polysulfone). Synthetic membranes are thick (>35 microns) with cross-sectional structures that are either homogeneous (e.g., AN69®, Hospal) or asymmetric (e.g., polysulfone). The asymmetry refers to a two-layer structure with an inner thin layer that regulates solute removal and a thick supporting stroma. Synthetic membranes can be either high flux or low flux.
Most modern high-flux dialyzers are relatively equivalent in their performance and safety, so key factors in choosing a dialyzer for an individual patient may include dialyzer clearance and biocompatibility.
DIALYZER CLEARANCE
Most dialysis membranes in use today are high-flux membranes with high diffusive and convective clearances and high ultrafiltration coefficients. Convective clearance is more relevant for middle and large molecules such as beta-2 microglobulin. All dialyzer manufacturers provide in-vitro clearance values for various molecules of clinical relevance at various blood and dialysate flow rates. In-vivo clearance values, however, are typically 10-15% lower than the in-vitro values. The relationship between clearance and the dialyzer surface area is not linear and relatively little improvement in clearance is seen beyond 2 m2 surface area. In a patient with inadequate clearance, increasing time on dialysis, optimizing blood and dialysate flow rates, using appropriately sized access needles, optimizing anticoagulation, and ensuring a properly functioning vascular access should be attempted before switching to a larger dialyzer in a patient with inadequate clearance. All manufacturers offer dialyzers of various membrane surface areas to match the size and needs of patients.
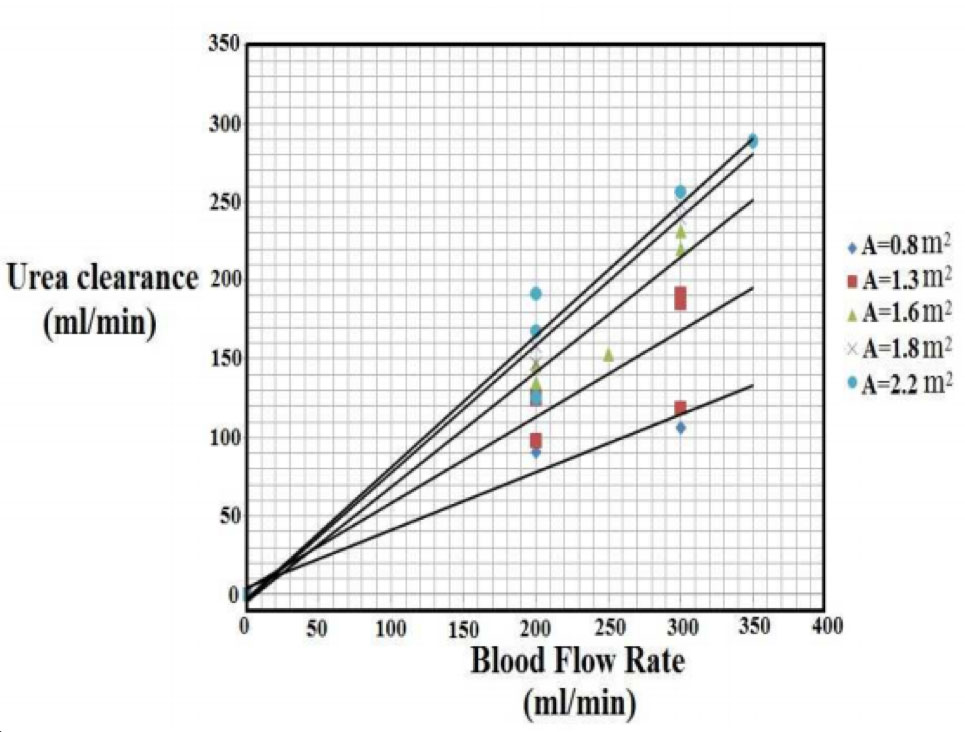
(Clearance values of hollow fiber dialyzer with membrane from polysulfone material for different areas1)
BIO- AND HEMOCOMPATIBILITY
During a hemodialysis treatment, activation of clotting factors and platelets results in thrombosis in the dialyzer. Activation of the complement system, with consequent activation of leukocytes can lead to:
- Acute intra-dialytic pulmonary hypertension
- Chronic low-grade systemic inflammation
- Leukocyte dysfunction
All dialysis membranes activate complement and leukocytes to some extent, but unmodified cellulosic membranes are potent complement and leukocyte activators and are generally considered bioincompatible.
In addition, the generation of bradykinin in the presence of a dialysis membrane with an anionic surface and accumulation of the bradykinin in plasma can cause anaphylactoid reactions in the presence of ACE inhibitors.
Early disposable hollow-fiber dialyzers were shipped filled with a formaldehyde solution to maintain sterility. Later, dialyzers were sterilized with ethylene oxide (ETO) and shipped dry, but the polyurethane potting material used in hollow-fiber dialyzers can act as a reservoir for ETO. Residual ETO can diffuse into the blood during dialysis, bind to plasma proteins, and induce antibody formation, leading to intradialytic anaphylactoid reactions, so ETO has now been largely replaced by alternative sterilization methods, such as steam and irradiation.
The decision to prefer one dialyzer brand over another may include additional factors such as the overall cost of the dialysis disposables, price discounts, reliability of the supply chain, and satisfaction with customer service.
Optiflux series (Fresenius Medical Care North America) and Revaclear (Baxter) dialyzers are the most commonly prescribed dialyzers in the U.S. with a market share of 74% and 17%, respectively.
NEW TECHNOLOGY MAY OFFER ADVANTAGES FOR DIALYZERS IN THE FUTURE
There have not been many advances in dialyzer membranes and designs since the introduction of high-flux synthetic membranes a few decades ago. Some of the changes in the dialyzer membranes and designs currently being investigated include:
- Addition of membrane surface modifications to improve biocompatibility and to reduce the risk of clotting; additives such as vitamin E, heparin and various surface modifying agents are being tested for this purpose
- Membranes with middle or high molecule weight cut-off to improve middle molecular clearance, albeit with increased loss of albumin during hemodialysis
- Manipulation of the fiber geometry to increase internal filtration to improve middle molecule clearance by convection
- Mixed matrix membranes using materials such as activated charcoal sandwiched between the internal and external lamina of the hollow fiber to improve toxin removal by adsorption
- Use of lightweight and environmentally friendly materials to reduce shipping and disposal impact on cost and the environment
SUMMARY
Most dialyzers in use today are high-flux and have similar clearance performance. Every dialysis facility must have options for patients with known hypersensitivity reactions to certain dialyzers. Dialyzers with different membrane materials and/or sterilization techniques should be available. Today, steam and gamma radiation sterilization are preferred to reduce the risk of allergic reactions associated with the use of ethylene oxide.
Additional articles to consider related to this topic:
- Hemodialysis (HEMO) Study Group. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002 Dec 19;347(25):2010-9. PubMed PMID: 12490682.
- Membrane Permeability Outcome (MPO) Study Group. Effect of membrane permeability on survival of hemodialysis patients. J Am Soc Nephrol. 2009 Mar;20(3):645-54. PMID: 19092122
- Performance of hemodialysis with novel medium cut-off dialyzers. Nephrol Dial Transplant. 2017 Jan 1;32(1):165-172. PubMed PMID: 27587605
- Results of the HepZero study comparing heparin-grafted membrane and standard care show that heparin-grafted dialyzer is safe and easy to use for heparin-free dialysis. Kidney Int. 2014. PubMed PMID: 25007166.
References
- Albert E. Yousif, Farah M. Abdul-Kareem, Ali J. Mudhaffer. A Comparative Study of the Physiological Parameters and Efficiency of the Various Types of Hemodialyzers. American Journal of Bioscience and Bioengineering. Vol. 3, No. 2, 2015, pp. 8-16. doi: 10.11648/j.bio.20150302.11



