
A COMPREHENSIVE PROGRAM FOR DISASTER MANAGEMENT | FMCNA
Fresenius Medical Care North America (FMCNA) takes a strategic and comprehensive approach to disaster management. In emergency situations, the Disaster Response Team (DRT) is deployed to work with local teams and ensure continuity of care for all patients. Mobilizing a local command center, the DRT begins by supporting FMCNA employees with food, water, shelter, and transportation so they in turn can care for patients. A focus on advance preparedness, clear communication with patients, efficient supply delivery, and well-trained volunteers are just some of the many factors that drive successful disaster management.
Unprecedented natural disasters plagued North America in 2017. Three hurricanes inflicted historic losses and costs for the areas they struck. California experienced its most destructive wildfire season on record. A 7.1 magnitude earthquake in Mexico City was the deadliest quake to hit that country in more than 30 years.
Patients living with end-stage renal disease (ESRD) depend on power and water for life-sustaining dialysis treatments. If they don’t have access to the right foods or consume unpurified water, missing dialysis treatments for just a few days can be dangerous. If dialysis treatments are interrupted for a prolonged period, ESRD patients become very sick and can potentially die.
FMCNA deploys its DRT to ensure continuity of care in these situations. The DRT assesses the condition of roads and infrastructure as well as the availability of power, filtered water, and supplies such as dialyzers, concentrate, and medications. These essentials are challenged when there are downed trees, impassable roads, damaged buildings, lack of power, compromised water supplies, disruption in Internet connections, and telephone communication issues.
Before Disaster Strikes
To stay prepared, FMCNA conducts mock disaster drills that include information technology, human resources, engineers, and medical professionals. Patients’ emergency contact information is confirmed each quarter. The DRT maintains relationships with key local, regional, and national entities— emergency operation centers; federal, state, and local governments; first responders; volunteer organizations; utilities; and businesses—so when a disaster strikes, critical needs are prioritized for patients receiving dialysis treatment.
“Because of our strong partnership with the Centers for Medicare and Medicaid Services, after Hurricanes Irma and Maria, we were able to assist with the evacuation of 89 patients from St. Thomas and open a newly constructed clinic in a matter of days—a process that typically takes 90 days. This collaboration and fast action made a remarkable difference in these patients’ lives.”
– Cameron Lynch, Senior Vice President of Government Affairs
Some natural disasters can be anticipated. In those cases, FMCNA’s Incident Command operations are activated in advance with representatives from across the company on regular calls to ensure the safety of employees and patients. If it is not possible to establish these ahead of a disaster, the team mobilizes as soon as possible following the event. During the 2017 hurricane season, the team held daily calls from August 23 until November 22, from Harvey to Irma to Maria, to organize efforts across the organization.
Of critical importance is the need to communicate facility closures with patients, how they can prepare, and where they can access current information. FMCNA schedules as many patients as possible before an anticipated storm to ensure continuity in treatment, often adding extra shifts to cover all patients. Patients receive emergency packets that include a three-day renal diet, a care transition report, a labs and medication list, and the patient emergency number, a 24-hour toll-free line.
“Our Disaster Response Team mobilizes well before a storm hits to ensure plans for continuity of care for our patients, and support and safety for our employees. We contact all of our patients immediately after a storm and conduct well visits if needed to assess their needs.”
– Bob Loeper, Vice President of Operations Support and Business Continuity/Disaster Response
Locating and Caring for Employees and Patients
Mobilizing local Command Centers is the backbone of disaster response operations. Leadership from outside the impacted area is brought in to run the Command Centers, enabling local leadership to focus on clinic operations. Command Center staff handle logistics, including accounting for all patients and employees and arranging for the distribution of food, personal generators, and other necessary supplies.
When the hurricanes hit Puerto Rico, the couriers hired by Spectra Laboratories were sometimes the first to make contact with isolated facilities that had no phone or Internet connections. In addition to lab supplies, they delivered food, water, and other necessities to staff and patients. Spectra also expanded its services on the island to handle patients from competitors’ labs that had been destroyed.
“I can’t say enough about our staff. They are genuinely caring, passionate, resilient, and empathetic–everything we’d ever expect from a caregiver.”
– Bill Valle, Chief Executive Officer
FMCNA’s approach to disaster response starts with caring for employees. Essentials such as food, water, fuel, medicine, transportation, and shelter are provided to staff so that they in turn can deliver care to patients. The first plane chartered following Hurricane Maria had 14 pallets of food and supplies for patients, employees, and their families, and the process continued for four to five weeks.
Employees in these situations go above and beyond to care for patients’ overall well-being. In Puerto Rico, employees bought toys and coloring books for children coming into clinics with their family members. They also purchased shoes for patients and families and used hot plates to make warm meals when patients came in for their treatment. When the clinic manager in Aransas Pass, Texas, learned that a patient was sleeping on cushions after Hurricane Harvey destroyed his bed, she found a staff member to donate a bed—and then, with the help of her colleagues, delivered the bed to him.
Volunteer supplemental staff was put in place to provide relief to local teams. After Hurricane Maria, dozens of FKC employees volunteered to go to Puerto Rico to relieve local staff who had been working nonstop despite their own difficult circumstances. In addition, for months, Command Center leaders rotated every week or two between the US mainland and Puerto Rico.
“We didn’t say no to any patient. Even if they are not from FKC, we dialyze all the patients here. I’m proud to be a Fresenius employee. What they say, they do.”
– Miguel Neris, Clinic Manager, Miami
“They’re my friends. I owe them my life. That’s it.”
– Thomas King, patient
Locating patients is often a challenge following a disaster. Many will wait out the storm at the home of a family member or friend in another city, transferring clinics in the short term. Some choose to permanently relocate to a new city. In both instances, the “home” dialysis center is not always notified. Figure 1 shows the difference in the number of patients who were treated in August 2017 and left for the mainland following the hurricanes compared to the same period in 2016. The severity of the storms in 2017 had an impact on the patient population.
In other instances, patients can be found, but transportation is a challenge. After Hurricane Harvey flooded Houston, FMCNA partnered with a Duck Boat (amphibious vehicle) company in Mobile, Alabama, to transport stranded patients to clinics. During the hurricanes in Texas and Florida, the Fresenius Health Partners Care Navigation Unit came forward to help patients arrange rides to their doctors’ appointments, including those beyond their dialysis treatments. After the earthquake in Mexico City, FMCNA created bus routes to operating clinics.
Figure 1 | Number of dialysis patients who left Puerto Rico for the mainland in August to October 2016 and 2017.

Water
A typical dialysis treatment requires roughly a bathtub full of specially prepared dialysis solution to clean one patient’s blood. In the first 30 days after Hurricane Maria struck Puerto Rico, water tanker trucks had to deliver water every other day to keep the cistern full. With the shortage of water came the need to identify immediate water-saving solutions to maximize the number of patients who could be treated. No patient would be turned away, even those from competitors’ clinics that were closed. To accommodate the demand, the dialysate flow rates and treatment times had to be reduced, which had the benefit of allowing more patients to be treated in a given day.
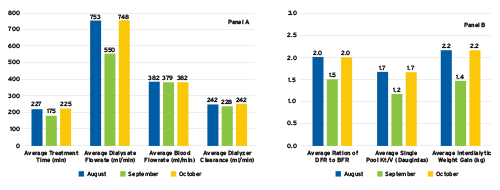
Figure 2 (Panel A) shows average dialysis parameters in Puerto Rico during the last week of each month. Average treatment time and dialysate flow rate (DFR) were reduced by about 25 percent in the last week of September to conserve water. The average blood flow rate (BFR) remained constant, and the ratio of DFR to BFR fell by about 25 percent. The reduced dialysate flow rate has minimal effect on dialyzer clearance because the ratio of DFR to BFR remained at or above the minimum recommended Autoflow setting of 1.5X.
The downside of shortened treatments and reduced dialysate flow rates is reduced dialysis adequacy, as shown in Panel B. Despite the need to reduce water usage in Puerto Rico, the average Kt/V remained slightly above the minimum recommended value of 1.2 per the CMS Quality Incentive Program. Furthermore, by the end of October, the adequacy results had rebounded to prior values.
While Kt/V is a measure of toxin removal, another concern is removing water so patients do not become overloaded with fluid, which can increase blood pressure and cause stress on the heart. If patients miss treatments, one would expect that the weight gain between treatments would be higher than normal, necessitating a longer treatment time. However, Panel B of Figure 2 shows that the interdialytic weight gain actually went down immediately following the hurricane, demonstrating that patients were drinking less due to the lack of municipal water. That reduction in fluid intake made it possible to safely remove fluid from patients despite the shortened treatment times.
Figure 2 | Impact of hurricane on dialysis parameters (data from last week of each month)
Power and Internet
Intermittent power and network disruption can present many challenges, including outages in the Chairside application used to manage patient treatments. Labs and orders are not always visible, and electronic documentation of doses given is not always possible. Likewise, the ability to receive faxes, including those from Spectra with lab results, can be affected.
To mitigate and prepare for these challenges, FMCNA responded by delivering specialized daily reports to clinics via e-mail to be accessed from a sister clinic with better connectivity at any time of day. These reports were designed to make it easy for facilities to verify data for the latest HGB labs and Mircera doses, which were used to calculate the new prescribed doses.
The lack of municipal electricity in Puerto Rico meant patients who normally used continuous cyclic peritoneal dialysis cyclers at their homes were quickly using up their backup supplies of continuous ambulatory peritoneal dialysis (CAPD) fluid, normally used only when there is a brief equipment issue or a patient is traveling for a day or two. To address this need, Renal Therapies Group (RTG) arranged for giant cargo planes to deliver needed CAPD supplies.
Coordinating Care
As a vertically integrated company with a focus on coordinated care, FMCNA has the ability to come together during a disaster and take care of patients. During the 2017 hurricane season, there were countless ways FMCNA collaborated across business units to ensure that every patient received the care they needed—from dialysis services to products to laboratories to prescriptions and beyond. This coordinated care extended beyond the four walls of a clinic, taking advantage of pre-established connections with government agencies or forging new partnerships to get much-needed supplies.
Meet Our Experts
Kate Dobbs
Senior Vice President of Marketing and Communications, Fresenius Medical Care
Kate Dobbs leads FMCNA’s marketing and communications team, overseeing marketing and brand strategy, public relations, employee communications, medical office communications, community relations, and digital strategy. She holds a master’s degree from Regis University and a postgraduate certificate in sustainable business from the University of Cambridge.
Norma Ofsthun, PhD
Vice President, Data Analytics, Fresenius Medical Care
Norma Ofsthun leads FMCNA’s clinical data analytics team and chairs the company’s Data Governance Program. She formerly worked in membrane-related research and development for Baxter Healthcare and holds her doctorate in chemical engineering from the Massachusetts Institute of Technology.



