
Water Purity in Hemodialysis
DOES TAP WATER MEET THE REQUIREMENTS?
During hemodialysis (HD), patients are exposed to copious volumes of dialysis fluid consisting of municipal or tap water. Tap water is obtained from either groundwater (wells and springs) or surface water (lakes, ponds, rivers, and other surface reservoirs). Groundwater usually contains fewer organic materials but more inorganic ions (e.g., iron, calcium, magnesium, and sulfate). Surface water is usually more contaminated with industrial wastes (microorganisms, fertilizers, pesticides, and sewage).
For tap water to be consumable, the Environmental Protection Agency (EPA) has set forth enforceable national primary drinking water regulations for municipal water based upon known toxicities and available technology to identify and remove contaminants.1 Notably, though, the safety standards for drinking water are not the same as those for dialysis-grade water2—in fact, they are much lower.
The relevant water standards for dialysis are established by the American National Standards Institute/Association for the Advancement of Medical Instrumentation (ANSI/AAMI). 3,4 They state that dialysis fluid must meet the minimum quality acceptable for routine hemodialysis, but the committee recommends using ultrapure dialysis fluid even for routine hemodialysis—underscoring the importance of appropriately treated water for use in dialysis.
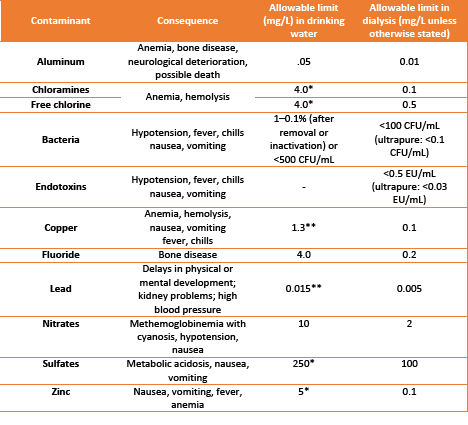
A comparison of allowable limits for both chemical and microbial contaminants is provided in Table 1. In addition to restricting contaminants, ANSI/AAMI also specifies the maximum allowable limits of electrolytes in the dialysate water (Table 2).
WHY IS DIALYSATE PURITY SO IMPORTANT?
Water for dialysis requires a higher level of purity than drinking water for a number of reasons:5,6
- The average volume of liquids consumed by a given individual is about 2 L/day, making the exposure level relatively low. In contrast, dialysis patients have a high exposure as they come into direct contact with over 200 L of dialysis fluid per treatment, at least three times per week.
- Drinking water allows the liquid to be processed through the gut and liver, where contaminants are inactivated or removed before absorption into the blood. With dialysis fluid, water comes into direct contact with patients' blood across the dialyzer membrane instead of the gut. Especially small molecules can freely diffuse across the membrane into the blood. Therefore, it is crucial that water being used for dialysis is adequately and appropriately treated before coming into direct contact with the patient.
- Finally, most patients on dialysis have little to no kidney function. The kidneys may compensate for higher intake of some substances from food and drink that would otherwise build up in the body. Dialyzing with pure water prevents exposure to substances that cannot be effectively eliminated from the body.
WHAT ARE POTENTIAL ADVERSE EFFECTS OF CONTAMINATED WATER?
Exposure to improperly treated water dialysate can result in both acute and chronic problems (Table 1). Although acute reactions are usually clinically evident and can be treated as they occur, chronic issues resulting from inadequately purified water can be missed and go untreated for long periods of time. This may lead to compounding of symptoms following each exposure and increased risks of morbidity and mortality.
PORTABLE WATER PURIFICATION SYSTEMS FOR HOME HEMODIALYSIS
Adequate water purification is available for patients dialyzing at home. There are currently two options to purify water at home:
- Compact reverse osmosis (RO) devices use the same technique as the dialysis units and provide ANSI/AAMI-quality water in real-time during dialysis. However, some plumbing modifications for typical home use are often needed for this method. Dialysis is then performed by a machine similar to in-center machines.
- Batch water purification devices prepare a batch of dialysate from tap water that can be used over several days. The system uses a smaller, portable home dialysis machine and employs much less water and lower dialysis flows than conventional dialysis. The system is fully portable and no major modifications to the home are needed. Additionally, the system can use water bags when travelling.
Home water purification is an active field of research for even more efficient and innovative options7,8 including sorbent-based technologies with continuous regeneration of small volumes of municipal water in closed-loop systems.9
ULTRAFILTRATION AND DIALYSIS
Even though dialysis uses large amounts of ultrapure water to remove accumulated metabolites and waste products, this water is not perfused into the patient. On the contrary, hemodialysis uses negative pressure to ultrafiltrate water across the dialyzer from the body to compensate for the impaired water removal by the kidneys. Ultrafiltration (UF) aims to reduce the patient’s fluid overload (FO) and return to the prescribed dry weight (DW) or slightly below.9 In addition to the absolute amount of fluid removed, the rate of removal (ultrafiltration rate, UFR) is important. As fluid is removed from the blood compartment, vascular or plasma refill occurs by shifting fluid from the tissues and organs into the vasculature to maintain blood volume. A slow UFR can prevent target weight attainment, which may lead to FO11,12. A fast UFR may cause a severe reduction in blood volume, resulting in intradialytic events.
To prevent the latter, the Centers for Medicare & Medicaid Services (CMS) proposed a maximum UFR of 13 mL/hr. Although appropriate for many, the UFR should be optimized for each patient through close monitoring during dialysis. Blood volume monitoring devices provide information on how the patient is tolerating the dialysis session by showing the relationship between the UFR and the vascular/plasma refill rate. In some instances, the excess water may not be adequately removed during one session, and longer or additional dialysis sessions are needed to ensure that the patient reaches the dry weight.
SUMMARY
Tap water contains contaminants that may not be harmful through ingestion but cause harm to the hemodialysis patient if not inactivated or removed. Thus, tap water must be appropriately and adequately purified prior to its use for dialysate preparation. This can be achieved in the dialysis center or the patient's home. While dialysate is needed for the removal toxins and waste products it does not enter the body. Adequate UF is pivotal to the patient's overall fluid management. Close attention must be paid to the appropriate amount of fluid removal as well as to balancing the UF rate with the patient's vascular refill to ensure reaching the dry weight while preventing intradialytic symptoms.
References
- Concepcion DB. Water treatment: The largest syringe used in dialysis. Nephrol News Issues. 2017;31(3):26-28. www.ncbi.nlm.nih.gov/pubmed/30399280
- Selected EPA-registered Disinfectants.
- Association for the Advancement of Medical Instrumentation. ANSI/AAMI 11663: 2014 Quality of dialysis fluid for hemodialysis and related therapies. Arlington, VA: AAMI.
- Association for the Advancement of Medical Instrumentation. ANSI/AAMI 13959: 2014 Water for hemodialysis and related therapies. Arlington, VA: AAMI.
- Payne GM, Curtis J. Water Treatment for Hemodialysis: What You Must Know to Keep Patients Safe. Nephrol Nurs J. 45(2):141-168. www.ncbi.nlm.nih.gov/pubmed/30303637
- Payne G. Hemodialysis: Water Treatment. In: Counts C, ed. Core Curriculum for Nephrology Nursing: Module 3 Treatment Options for Patients with Chronic Kidney Failure. 6th ed. Pitman, NJ: American Nephrology Nurses’ Association;2015:101-113.
- van Gelder MK, Mihaila SM, Jansen J, Wester M, Verhaar MC, Joles JA, Stamatialis D, Masereeuw R, Gerritsen KGF. From portable dialysis to a bioengineered kidney. Expert Rev Med Devices. 2018;15(5):323-336.
- Agar JWM. Green Dialysis: The Environmental Challenges Ahead. Semin Dial. 2015;28(2):186-192. www.ncbi.nlm.nih.gov/pubmed/25440109
- Zoccali C, Moissl U, Chazot C, Mallamaci F, Tripepi G, Arkossy O, Wabel P, Stuard S. Chronic Fluid Overload and Mortality in ESRD. J Am Soc Nephrol. 2017;28(8):2491-2497. www.ncbi.nlm.nih.gov/pubmed/28473637
- Chou JA, Kalantar-Zadeh K. Volume Balance and Intradialytic Ultrafiltration Rate in the Hemodialysis Patient. Curr Heart Fail Rep. 2017;14(5):421-427. www.ncbi.nlm.nih.gov/pubmed/28803369
- Flythe JE, Xue H, Lynch KE, Curhan GC, Brunelli SM. Association of mortality risk with various definitions of intradialytic hypotension. J Am Soc Nephrol. 2015;26(3):724-34. www.ncbi.nlm.nih.gov/pubmed/25270068
- Assimon MM, Flythe JE. Rapid ultrafiltration rates and outcomes among hemodialysis patients: re-examining the evidence base. Curr Opin Nephrol Hypertens. 2015;24(6):525-30. www.ncbi.nlm.nih.gov/pubmed/26371525
*Unenforceable maximum contaminant level goal (secondary standard).
**Action level at 90th percentile.
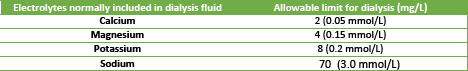
Maximum allowable levels of electrolytes in dialysis water3,4



