
Value Based Care and the Evolution of Health Payment Models
By Dr. Terry Ketchersid
The shift to value based care has been a positive one for both patients and the healthcare system. But, it’s left many physicians, particularly nephrologists, with a lot of questions about how they can be reimbursed for their services. In this article, we aim to demystify the ever-changing reimbursement landscape for nephrologists.
MACRA and the Nephrologist
Enacted in 2015, the Medicare Access and CHIP Reauthorization Act (MACRA) did three important things from the perspective of the nephrologist:
- Repealed the sustainable growth rate (SGR), eliminating the flawed formula used to establish annual updates to the Medicare physician fee schedule (PFS)
- Sunset the three stand-alone CMS incentive programs (Physician Quality Reporting System or PQRS, Meaningful Use and the Physician Value-Based Payment Modifier or VBPM)
- Created the Quality Payment Program (QPP), which replaces the programs outlined above in 1 and 2
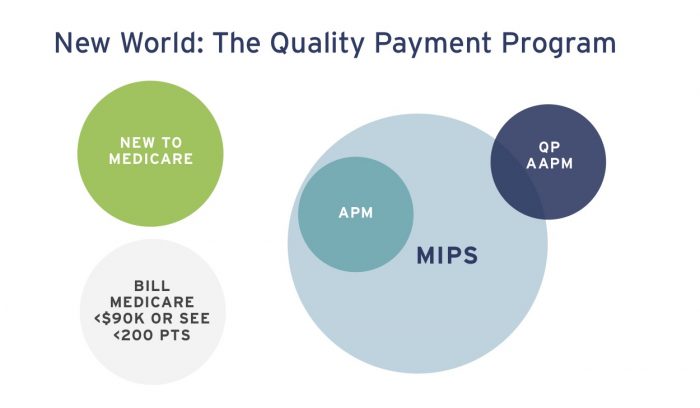
The QPP, now in its second year, represents a generational change with respect to the way Medicare pays physicians. The QPP effectively creates two physician payment tracks. Unless you are excluded, due to low volume or because it is your first year billing Medicare, you are either subject to the Merit-based Incentive Payment System (MIPS), or you are a Qualifying Participant (QP) within an Advanced Alternative Payment Model (Advanced APM or AAPM).
Fee Schedule Impact
Beginning in 2017, the QPP directly impacts your future Medicare physician fee schedule. With the repeal of the SGR, MACRA creates a 0.5% PFS increase for a couple of years and then freezes the fee schedule for several years. During the freeze, the published fee schedule represents the starting point, but what you are actually paid depends on whether you are subject to MIPS or participating in an Advanced APM. If you are subject to MIPS, your MIPS score during the performance year determines what percentage of the PFS you will receive during the payment year. Those subject to MIPS in 2018 will receive between 95 and 105% of the PFS in 2020. Where you lie on this continuum is dictated by your 2018 MIPS score. This +/- 5% corridor expands to +/- 7% in payment year 2021 and to +/- 9% in 2022 and beyond.
MIPS
MIPS uses components of the three CMS incentive programs sunset by MACRA, adds a fourth new category, and rolls all four up to provide each practitioner with a MIPS score. That score on a scale of 0-100 is used to compare the performance of all physicians across the country. Physicians with a MIPS score equal to the national average in 2018 will receive the published PFS in 2020 without an adjustment. Those with a MIPS score exceeding the average will realize an upward adjustment in their 2020 fee schedule, while those with a MIPS score below the average will face a downward adjustment. It’s this differential payment to physicians, based on their MIPS score, which makes the QPP such a dramatic departure from prior Medicare physician reimbursement schemes. In essence, MIPS is a zero sum game, where the high performers are paid with funds collected by penalizing the poor performers.
MIPS Categories
Most of the MIPS categories are familiar to nephrologists:
- Quality looks just like PQRS—the principle difference is that in MIPS, the quality category is pay-for-performance
- Improvement Activities is new, but appears to be the most simplistic aspect of MIPS
- Advancing Care Information is essentially Meaningful Use, but this version is easier to navigate than the original version
- Cost uses parts of the resource side of the Physician Value-Based Modifier

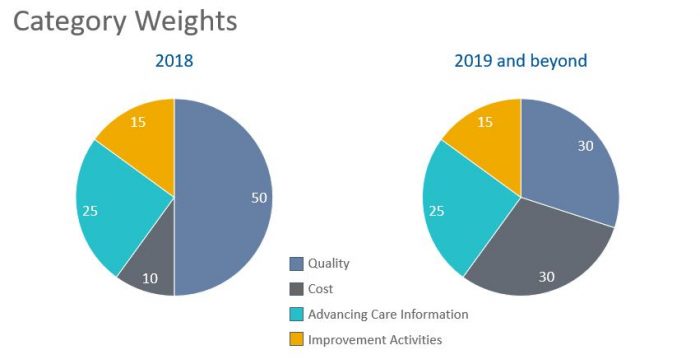
At a high level, you receive a sub-score within each MIPS category, and those four sub-scores are added together to generate your MIPS score. Additional details on how each category works can be found on the QPP website or visit Acumen Physician Solutions’ blog series for insight. In addition, the relative weights for each category will change next year as noted below.
Importantly, there are three groups of providers excluded from MIPS:
- New to Medicare (recently matriculated nephrology fellows who have not billed Medicare in the past are excluded for one year)
- Low volume threshold (you see fewer than 200 Medicare beneficiaries during the year OR collect less than $90,000 from Medicare during the year)
- You are a Qualifying Participant within an Advanced APM (like an ESCO).
Alternative Payment Models
An alternative payment model (APM) is best described as a system for reimbursement that provides additional compensation as an incentive for the delivery of higher quality and more cost-efficient health care. There are dozens of APMs available today. The APMs of interest to the nephrologist fall into one of two categories; Advanced APMs, or so-called MIPS APMs. Advanced APMs are distinguished by the presence of three criterion:
- Require participants to use Certified EHR Technology
- Base payments for services on quality measures comparable to those in MIPS
- Require participants to bear more than nominal financial risk
Each year, CMS will publish the list of APMs that meet the criteria to be classified as an Advanced APM. That list includes the two-sided risk ESCO. Today Fresenius operates 24 of the 35 two-sided risk ESCOs. Last year all physicians participating in those ESCOs were determined to be Qualifying Participants. QPs were excluded from MIPS in 2017, and in 2019 they will receive a lump sum payment equivalent to 5% of their 2018 Part B book of business.
MIPS APM
As a nephrologist, you may participate in a MIPS APM. The Medicare Shared Savings Program (MSSP) track 1 ACO is the most common MIPS APM. Fulfilling the MIPS requirements is substantially easier within a MIPS APM. Typically, the Advancing Care Information category within MIPS is the only category you are compelled to report for MIPS within a MIPS APM. The other three categories are either excluded or they are reported by the APM. While the MIPS APM does lessen the administrative overhead required to participate in MIPS, it’s important to recognize that all physicians within a MIPS APM receive the same MIPS score, and therefore all will see the same adjustment to their PFS during the payment year.
Summary
Last year, nephrologists began a new journey with respect to Medicare payment. The QPP represents a sea change which will see physician payment differentials based on performance within the program. CMS has created attractive financial incentives designed to increase participation in Advanced APMs like the ESCO. In conjunction with our nephrology partners, Fresenius recognized early success in the ESCO program, and we remain committed to actively participating in the national conversation as health care payment models evolve.
About Terry Ketchersid, MD
Dr. Terry Ketchersid is Senior Vice President and Chief Medical Officer for Fresenius Medical Care’s Integrated Care Group where he has clinical oversight over FMCNA’s value-based care initiatives and ESCO programs. He received his B.A. in chemistry from Austin College, his executive MBA from Duke University’s Fuqua School of Business and his MD degree from the University of Texas Southwestern Medical School.



