Bloodlines
INDICATIONS, SAFETY AND WARNINGS
Vascular access failure is one of the causes of hospitalization in dialysis patients, and access thrombosis is a leading cause of loss of access patency.1 In addition, vascular access complications can contribute to as much as 25% of all dialysis patient hospitalizations per annum with the vast majority due to thrombosis.1,2 Vascular access dysfunction is also costly, with vascular access care estimates reported at $1.8 billion annually.3
A vascular access surveillance program provides information clinicians can use to extend the lifespan of the vascular access through planning, coordination and elective corrective intervention. Such a program may reduce the frequency of urgent procedures resulting in the need for catheters or hospitalizations. According to KDOQI Clinical Practice Guidelines,4 “It has been shown that an aggressive policy for monitoring hemodynamics within AVG or AVF to detect access dysfunction may reduce the rate of thrombosis.”1
An effective surveillance program may allow the early detection of patient access dysfunction before the patient develops complications. Coupled with a program of elective stenosis correction, access thrombosis rates decline approximately 50-75%.4
Vascular access dysfunction may lead to patients being under-dialyzed, resulting in lower Kt/V and an increase in morbidity and mortality. Every 0.1 decrease in Kt/V is associated with 11% more hospitalizations and 12% more hospital days.1
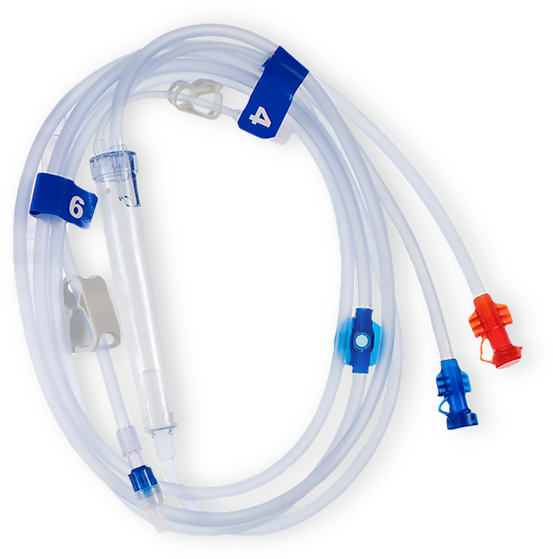
Through routine and consistent use of a vascular access surveillance program, staff may easily identify access dysfunction through a combination of physical assessment and intradialytic monitoring. A simple way to implement such a program is using the 2008® series hemodialysis machines with Access Flow feature and the CombiSet® True Flow bloodline with Twister device.
References
1. National Kidney Foundation, “NKF K/DOQI Guidelines: Clinical Practice Guidelines and Recommendations, 2006 Updates Hemodialysis Adequacy, Peritoneal Adequacy, Vascular Access.” Available: here. Pages 241-242, 273-301.
2. Rios, Danyelle et al, “Hemodialysis Vascular Access Thrombosis: The Role of Factor V Leiden, Prothrombin Gene Mutation and ABO Blood Group.” Clinica Chimica Acta, 412 (2011): 425-429.
3. Chang et al, “Intradialytic Hypotension and Vascular Access Thrombosis”. Journal of the American Society of Nephrology, 8 (2011): 1526-1533.
4. Sands, Jeffery, “Vascular Access Monitoring Improves Outcomes”. Blood Purification, 23 (2005): 45-49
RELATED PRODUCTS